By: Renee Murray, Camden Coalition of Healthcare Providers
Patient engagement strategies — particularly those that reflect whole-person care principles and support individuals living with social and medical complexities — are rising to the forefront as critical tools in a provider’s toolbox. Effective engagement strategies keep patients involved in an intervention, fostering a stronger relationship between provider and patient, and creating real potential for better health outcomes and better quality of life for the patient.
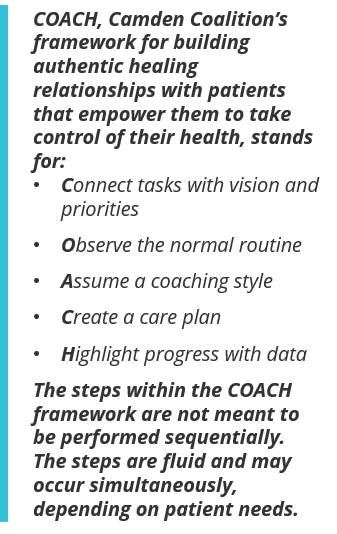
But, engaging individuals with complex health and social needs and empowering them to take control of their health can be challenging for many providers. The challenge was no different for the Camden Coalition, a multidisciplinary nonprofit working to improve care for people with complex health and social needs in Camden, NJ, and across the country. As our work with individuals with complex needs evolved, we found we were able to successfully engage individuals while providing care coordination to help them navigate the fragmented health care system. However, after patients completed our short-term intervention and no longer had our support, we often saw increased hospital utilization, as well as a general lack of understanding about how to complete everyday tasks like scheduling doctor appointments, setting up transportation, and/or accessing food resources. While we have not solved this problem fully, we have learned important lessons about coaching patients toward independence through the development of a new framework called COACH.
The Problem with the “Fix-it” Framework
It was clear that our Camden Core Model, which offers short-term, intensive case management, needed a different approach to sustaining patient engagement. When we started our work, we entered patients’ lives and did the fixing for them, not with them. We realized we needed to shift from having individuals trust us to get things done to building their own capacity. Changing our “fix-it” practice norm was easier said than done.
The inclination to fix patients’ problems had been ingrained in us as clinicians and social workers. However, fixing patients’ issues was not a long-term solution, and placing the full weight of problem-solving on our shoulders resulted in staff burnout across the organization. So, we asked our patients what they wanted. We learned that our patients did not just want “fix-it” solutions, but rather, they wanted strong, genuine relationships that validated their experiences and helped them navigate the health care system and manage their chronic conditions and social needs. This is how the COACH framework was born.
Building Authentic Healing Relationships through COACH
We understood the need for qualitative data to build a new patient engagement framework to support this strategic shift. A team of researchers from the Camden Coalition and Thomas Jefferson University partnered to conduct interviews with 30 former patients to gain insight into what was and was not working well in our intervention. The study findings pointed to the profound impact of the relationships between patients and care managers, and how these relationships can facilitate positive behavior change.
In fact, while describing their experiences with the Camden Coalition, study participants “spent the majority of time and emphasis recalling and describing the relationships formed with their care team members,” which were linked to increased “motivation to engage in and sustain active health management.” These are what we now call authentic healing relationships, and they form the core of our work. We created the COACH framework to help build and strengthen these relationships.
Authentic healing relationships are respectful, trusting, and non-judgmental partnerships between our care team and the patient. These relationships serve as the foundation for progress toward long-term health management. [COACH manual, pg. 3]
While authentic healing relationships anchor the COACH framework as the mode of service delivery, COACH is also informed by the key principles of trauma-informed care. To fully understand our patients and help address their needs, we need to unearth the many layers of complexity and life experiences that have brought them into our intervention. More often than not, trauma is one of those layers. COACH relies heavily on the elements of trauma-informed care to identify the root causes of poor health and begin the journey toward wellness.
The COACH Framework in Action
When we first met “Mr. Jones,” he was quiet and guarded. It took numerous engagement attempts for him to begin to trust us and accept the support we offered — a common effect of historical trauma. During our early home and community visits, we focused on learning about him, rather than imposing our own ideas about what we thought he needed. We asked questions to understand his living conditions, medication regimen, existing support systems, and process for managing his care. We facilitated conversations about his passions and joys, and developed insight into social determinants and other factors that were adversely impacting his health. Observing Mr. Jones’ normal routine is one step in building an authentic healing relationship.
From this observational vantage point, we were in the right position to then Assume a coaching style. Patients have varying levels of need. Some may also be able to navigate certain systems of care better than others. With this knowledge in hand, we assume a coaching style with an “I do, we do, or you do” approach. The goal is to eventually move all patient activities to a “you do” frame. Mr. Jones, for example, had difficulty identifying the first step in scheduling transportation for his appointment, so we assumed an “I do” coaching style by performing the task, modeling it for him, and walking him through the process. Over time, after helping him perform the task together through a “we do” approach, he was able to schedule his own transportation effectively, so we assumed a "You Do" approach to that aspect of his care. At another point in his care, Mr. Jones had a solid understanding of which medications were used for each of his chronic conditions, but would often be uncertain about the dosage and timing of them. Over time, after helping him perform the task of packing his pill box together, through a "we do" approach, Mr. Jones became more confident in packing his pill box on his own.
During our conversations with Mr. Jones, we uncovered his personal vision: He wanted to feel good enough to play with his grandchildren in the park and give back to his community by volunteering. We Created a care plan with him that reflected these goals, and throughout the intervention, we frequently discussed his overall vision and Connected it to the tasks that were necessary to reach that vision. To keep Mr. Jones motivated on his journey, we regularly Highlighted his progress with data that reflected his goals and priorities and celebrated successes along the way.
COACHing Others in Our Patient Engagement Philosophy
In our technical assistance work, we have shared our COACH philosophy with a variety of partners. We have trained organizations inside and outside of the health care sector, locally and across the country. For example, we have partnered locally with the Center for Family Services — a nonprofit that provides behavioral health, housing, advocacy, and support services to individuals and families in Camden — to deliver a series of COACH trainings aimed at encouraging community members to employ a more client-centered approach in their work. Representatives from a variety of service provider organizations that regularly engage with families and individuals in our Camden community participated in the training.
One key takeaway from our partnership with the Center for Family Services was that participants not only developed their own organizational patient engagement strategies, but were also able to form cross-organizational connections with peers doing similar work within the community. Throughout the six-month training period, participants discussed the struggles and joys of serving individuals with complex needs, and reflected on ways to support each other’s patient engagement work.
We also collaborated with Providence St. Joseph Health, a nonprofit health system serving low-income and vulnerable residents in a variety of states, including Alaska, California, Washington, and Montana. To date, we have delivered COACH training to 165 of their staff members. Providence St. Joseph Health is passionate about delivering patient-centered services that facilitate whole-person care, including addressing the social and behavioral health needs of their patients. Participant feedback in post-training surveys was overwhelmingly positive, with 81 percent of participants who completed training evaluations reporting that they would recommend the COACH training to others.
Conclusion
Our work is an iterative, challenging process. We are still learning how to better support our patients, and sometimes, despite our best efforts to build relationships, we are unable to help people. In some cases, they are not ready to help themselves Moreover, our experience has taught us that the more we can strengthen the connections between sectors and build ecosystems — local networks of organizations that collaborate to serve individuals with complex needs — the more health providers will be better equipped to address patient needs. In traditional health care, patients are often expected to look to providers for their expert opinion on what should be done to achieve better health. But our COACH engagement strategy changes that dynamic. COACH honors the patient's own capacity, enabling them to be actively involved in their health and wellness, rather than observing from the sidelines.
Renee Murray is Associate Director for Technical Assistance and Training at the Camden Coalition of Healthcare Providers.