By Scott A. Fields, MD, MHA, Chief Medical Officer, OCHIN
In January 2020, One Community Health decided to add virtual care to the tools it uses to treat predominantly underserved communities in a rural region on the border between Oregon and Washington. Initially, it planned a gradual implementation to conclude in late 2020. But by the end of February, COVID-19 had arrived in Oregon. Like other federally qualified health centers (FQHCs) across the country, One Community Health (OCH) had to adapt quickly to respond to the pandemic and expedite the transition to virtual care.
“Our number one goal was to minimize the risk of the virus spreading to our patients and staff, especially knowing that asymptomatic people can have the virus,” said Max Janasik, OCH’s CEO. “Virtual was a tremendous benefit, allowing us to continue to care for individuals without putting them at risk.”
OCH worked with OCHIN, a health technology nonprofit that specializes in support for local health centers and community clinics across the country, to successfully deploy MyChart Virtual Visits just two days after deciding to go live. OCHIN’s turnkey virtual care solution enabled the health center to radically transform its model of care delivery in the face of COVID-19.
Transforming Health Care Delivery During a Pandemic
For nearly 34 years, OCH has evolved its services to meet the complex needs of vulnerable patients. Today, the majority of its 15,000 patients are on Medicaid or are low income, which can make it difficult for them to miss work or arrange childcare to make it to their doctor’s appointments. Some households live long distances from OCH’s clinics, posing significant transportation challenges — especially in the harsh winter months. About half of OCH’s patients prefer Spanish as their primary language, including many seasonal farmworkers.
The ability to adapt and meet patients where they are has enabled OCH to steadily improve access to health care in these rural communities through new approaches, like a school-based clinic. Now, OCH is working to remove additional barriers and further improve health equity by enabling virtual care.
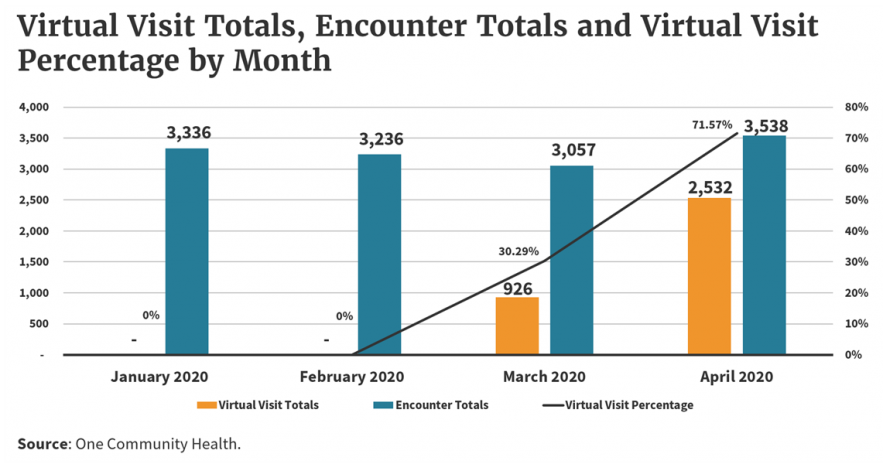
MyChart Virtual Visits feature a seamless Epic and Zoom integration that allows providers to easily schedule and conduct video or telephone appointments with patients — all within the secure and HIPAA-compliant MyChart portal that many patients are already familiar with. Once these new tools were live, Janasik engaged his leadership team to immediately convert as many in-person care appointments to virtual visits as possible. In just over one month since its adoption, more than 70 percent of patient visits at OCH have been completed virtually, with nearly 3,500 virtual encounters logged through April.
In the midst of the pandemic, this rapid transformation enabled providers to conduct COVID-19 screenings remotely and refer patients to the health center’s dedicated outdoor care tents for follow-up testing. As local concern about the spread of coronavirus mounted, the new “Tele-to-Tent” workflow at OCH helped minimize exposure for both patients and staff, conserve scarce personal protective equipment, and reduce the chance of COVID-19 entering the clinic where OCH continues to see expecting mothers and other patients with complex health care needs.
Overcoming the Hurdles of New Technology Adoption
While activating the new technology was relatively easy, OCH did have to work through some initial challenges in transitioning to this new model of virtual care. The first was ensuring that all its providers were trained and felt comfortable on the new platform. To accomplish this quickly, OCH leveraged its innovation team — a small internal working group that supports new technology deployments at the health center. One member of this team partnered with the clinic’s lead provider to do a live demonstration of a MyChart Virtual Visit at a provider meeting, so everyone could see how it works and how easy it is to register patients and launch visits.
The bigger challenge, according to Janasik, was bringing patients online. To accelerate this, OCH waived all out-of-pocket patient expenses for virtual visits for the first 30 days and made an upfront effort to engage and educate patients across a variety of communication channels. It used tools provided by OCHIN, such as MyChart bulk activation and WELL Health text messaging, to prompt patients to register with MyChart, in order to access the new virtual care platform. OCH promoted the service via email and social networking, and created a bilingual outbound calling team to guide patients through the set-up process over the phone. Patients can also find instructions and support on the virtual visits page of One Community Health’s public website, which includes a patient-centered orientation video.
This approach helped OCH achieve nearly a 50 percent increase in its total MyChart patient enrollment in a month. With a growing volume of patients now enrolled in MyChart, OCH providers can more easily communicate directly with their patients through a variety of messaging tools and utilize the newly enabled virtual visit capability to conduct video appointments for the first time.
By the end of April, the rapid adoption of virtual visits also enabled the health center’s medical and behavioral health services to return to pre-COVID patient volumes, despite a precipitous decline in non-coronavirus medical appointments nationally. Some long-term business challenges remain, such as reducing the billing complexity of virtual visits and ensuring that temporary federal waivers and reimbursements stay in place for health centers, even after the CARES Act and other emergency pandemic legislation expires. But Janasik says the quick roll out of these new virtual capabilities has helped fuel a lasting culture shift for OCH.
“We quickly realized that it doesn’t have to take a year to make change,’” Janasik said. “It’s hard to underestimate how empowering that is for improving an organization.”
Discovering the Long-Term Benefits of Virtual Care for Vulnerable Patients
MyChart Virtual Visits have helped OCH keep its most vulnerable patients, staff, and their families safe throughout the pandemic by limiting direct contact and exposure. But both patients and providers are also discovering long-term benefits and new use cases for virtual medicine, as a result of their first-hand experiences.
Two of the biggest advantages of virtual care for patients are reduced travel/wait times, and increased mobility and convenience. Many of OCH’s patients live in remote areas, sometimes more than 50 miles away from the nearest clinic. For elderly patients, those relying on public transportation, or anyone attempting to travel during severe winter weather, this can be an arduous and unsafe journey. Virtual care saves patients the trip and allows for more convenient scheduling of appointments between work, school, or childcare obligations. According to Janasik, many OCH patients have smart phones and cellular service, even when access to laptops and broadband are limited, and family members can provide helpful technical support to each other as well.
In one case, a 76-year-old woman who was recovering from a stroke at home was able to complete a comprehensive geriatric visit virtually, with some help from her son. He not only managed her technical set up for the appointment, but also held the phone while she performed daily activities so her provider could visually assess her progress and the safety set up of her home. Live video also simplified the review, organization, and refill process for her medications and helped foster a personal connection that reduced her feelings of social isolation.
Clinicians are benefiting from the streamlined functionality of virtual tools as well. Fewer no-shows and shorter transitions between appointments saves time and could help reduce potential burnout. At OCH, a short “Tech Check” process was implemented to further optimize the virtual visit experience. About 15 minutes prior to each appointment, medical assistants help virtual patients in troubleshooting any technical issues and ensure they are checked on time for their provider visit. Essential in-person care is still available when it is needed, but many providers now work at least partially from the safety of their own homes, while still enjoying visual access to their patients and close digital connectivity with their peers. For example, primary care providers at OCH use OCHIN’s secure instant messaging tools in Epic to provide real-time referrals and warm video introductions to a behavioral health consultant when patients need additional help managing their stress or anxiety.
“We’re really promoting our behavioral health team right now,” Janasik said. “We know that almost everyone is struggling with new levels of stress, given the restrictions and isolation of stay at home orders. The longer this persists without support, the higher the likelihood for increased emotional, physical, or substance abuse because people aren’t accustomed to living this way, and they need strategies for how to manage the tension before it boils over.”
Behavioral health care providers at One Community Health now complete all of their patient visits virtually, enabling continuity of care and additional support for patients during the COVID-19 pandemic. (Photo credit: One Community Health)
“We anticipate virtual visits becoming an essential new way for patients to access our behavioral health services, even when we reopen in-clinic visits,” said OCH’s Director of Behavioral Health Lucas O’Laughlin. “Patients appreciate the time and money (gas, time off work) savings afforded by virtual visits, particularly for low-income families where every hour worked is vital. We also see virtual visits expanding the geographies and patients we can serve. For instance, children and teens can access care from their schools, while minimizing missed class time. We can serve rural communities with our existing staff, without having to invest in physical buildings in remote areas. COVID-19 has really helped normalize virtual care, which we expect to have lasting positive effects on access and utilization.”
In addition to behavioral health, the health center has also just launched virtual care tools to conduct remote dental screenings, in order to help prioritize patients for emergency dental treatment or facilitate appropriate self-care at home.
“There are new use cases that we may not have planned for that we’re going to be discovering as people experiment with this,” Janasik said. “And that’s what I enjoy the most — when something you don’t anticipate has unique benefits that it offers the community.”
Scaling Virtual Care Nationally
The emergence of COVID-19 has created an unprecedented need, and opportunity, for innovative health care delivery. OCH is just one example of the growing number of health care providers nationally that are testing and refining the implementation of virtual care on the frontlines of the pandemic.
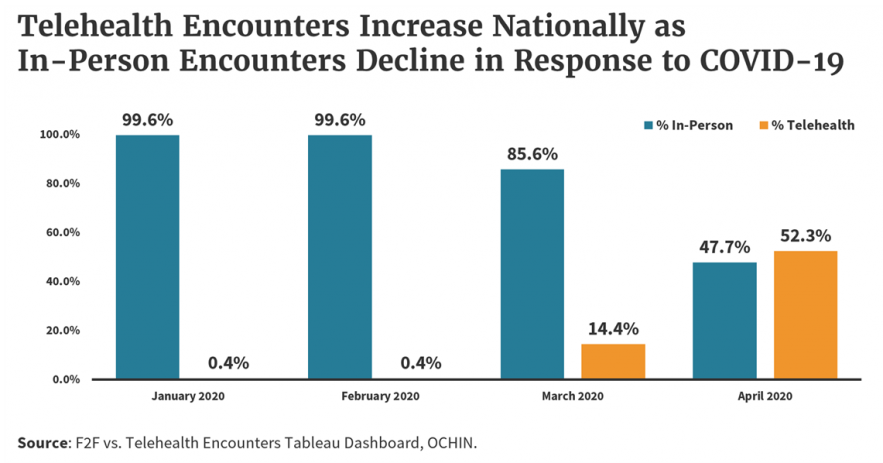
Across the OCHIN network, which includes more than 500 points of care in 47 states, more than half of all patient visits are now occurring virtually.
Telehealth encounters increased in volume from less than 1 percent in February of this year to more than 14 percent in March and more than 52 percent in April — totaling more than 348,000 virtual visits. This growth is expected to continue as both patients and providers discover the lasting benefits of virtual care, especially for improving health care access in underserved communities.