The payer who is at-risk for the health care costs of the population you serve can be a strong partner in designing enhanced care models for patients with complex needs and high costs. These organizations, whether private health insurers, Medicare or Medicaid plans, hospital systems, or accountable care organizations, likely have their own complex care programs and goals, as well as claims and utilization data useful in designing, measuring, and improving care. If you can demonstrate the value your enhanced care program has in helping them meet their goals, they may be interested in providing financial resources or in longer term innovative payment models.
The goal of this play is to help you develop the necessary partnerships.

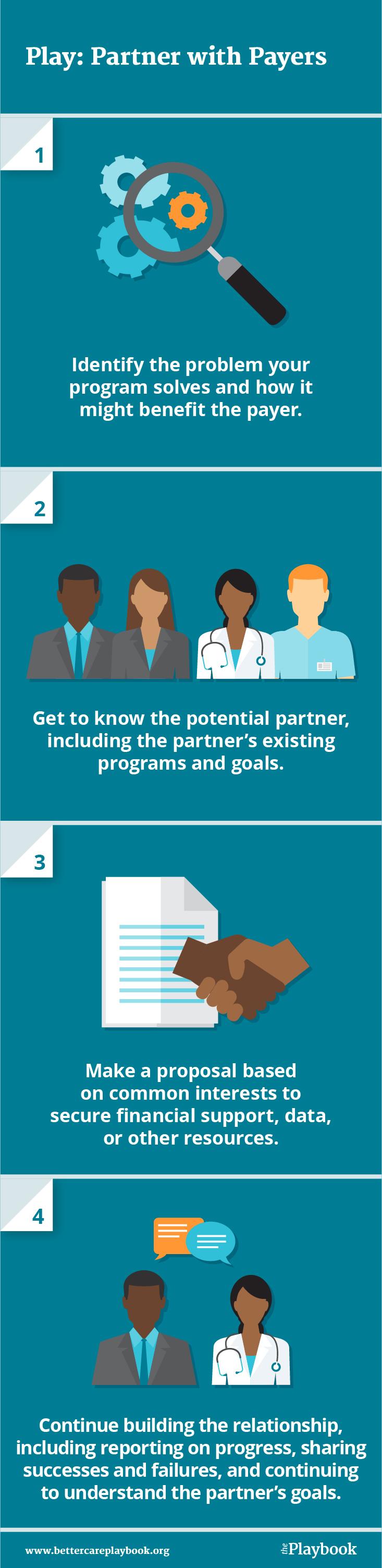
- Identify the problem your program solves and how it might benefit the payer.
- Get to know the potential partner, including the partner’s existing programs and goals.
- Make a proposal based on common interests to secure financial support, data, or other resources.
- Continue building the relationship, including reporting on progress, sharing successes and failures, and continuing to understand the partner’s goals.
- Start small and get your foot in the door by identifying an individual within the potential partner whom you can meet in person. If the payer has its own care management programs, consider reaching out to program leaders.
- Organize your own data, including initial information about how you see the problem of high health care utilization and poor quality among people with complex needs. If your program is further along, include key metrics on the population you serve and the results achieved.
- Make the business case, which may be based on financial returns or other interests. Understand the partner’s strategic priorities and how these might relate to complex care.
- If your goal is to access the partner’s data, be sure you think through which data you’ll need in a concrete way. Which measures? How frequently updated? To share for how long?
- Don’t forget to continue developing the relationship even if you form a successful partnership. Report back on how your work is going, and continue getting to know people within the organization personally.
For More Information
- Learn more about IHI's complex care efforts.
- Read more about Strategies for Partnering with Payers on the Care Redesign Guide.
- Learn about payer partnerships to improve care on the IHI blog.
- For more on the Better Care Playbook:
This play was developed by the Institute for Healthcare Improvement (IHI) based on their work in the Better Health and Lower Costs for People with Complex Needs collaborative, which ran from 2014-2017.


